Every day, millions of Canadians are managing diabetes, a condition that affects how the body regulates blood sugar, or glucose. In fact, Health Canada estimates more than 3.8 million Canadians aged one and older have diagnosed diabetes.
Understanding the causes, early warning signs, and treatment options for diabetes is essential to maintaining long-term health.
Whether you’ve just been diagnosed, are at risk, or have a family member with diabetes, learning the basics can help you take meaningful steps toward prevention and effective management.
In this article, we’ll explore the main causes of diabetes, the differences between its types, and how you can protect your health through early detection and proper care.
What Is Diabetes?
Diabetes is a chronic condition that occurs when the body cannot properly regulate blood sugar levels.
Normally, insulin, a hormone made by the pancreas, helps glucose (sugar) from food enter cells to be used for energy. When this process is disrupted, glucose builds up in the bloodstream instead of being absorbed by the cells. This leads to a spike in blood sugar.
If left unmanaged long-term, high blood sugar levels can result in the risk of serious diabetes-related complications such as heart disease, vision loss, and kidney problems, according to Diabetes Canada.
Is Anyone At Risk?
Diabetes is not limited to one group. Anyone can develop it, regardless of age, gender, or background. However, certain factors like family history, ethnicity, and body weight can increase the likelihood. This may include:
- People of Indigenous, South Asian, African, and Hispanic descent are at a higher risk.
- Adults over the age of 40 are more likely to develop Type 2 diabetes.
- Sedentary lifestyles, unhealthy diets, and excess weight contribute significantly to rising cases.
In short, while some risk factors can’t be changed, many can be managed through healthy habits and regular screenings.
Types of Diabetes
There are three main types of diabetes: Type 1, Type 2, and gestational diabetes, along with a precursor stage known as prediabetes. Each type affects how your body uses insulin differently.
Type 1 Diabetes
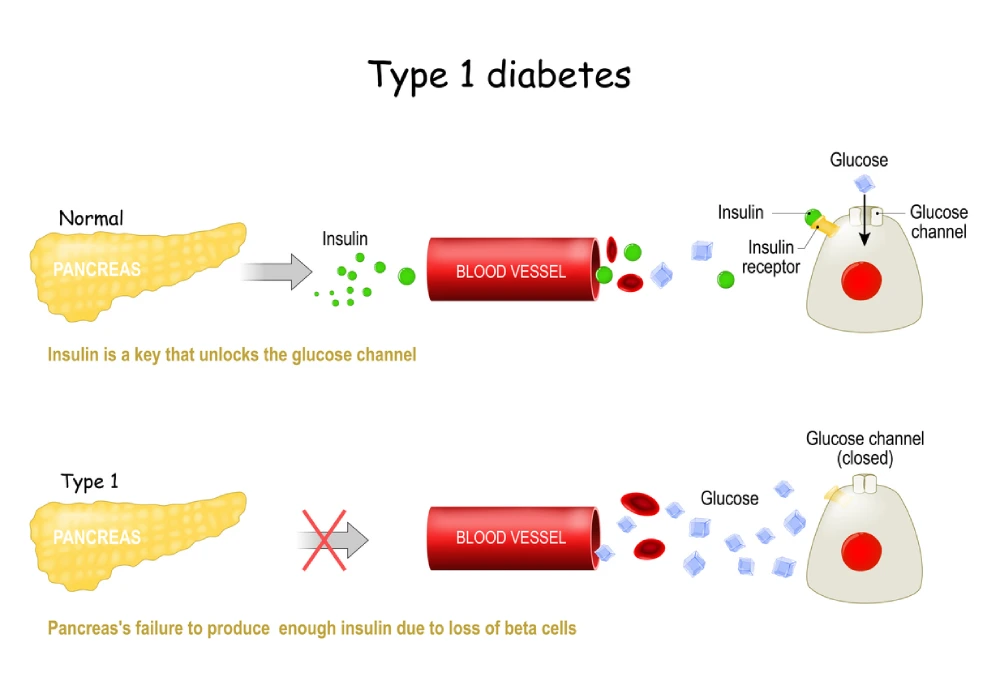
Type 1 diabetes occurs when the immune system mistakenly attacks insulin-producing cells in the pancreas. As a result, the body produces little or no insulin, requiring daily insulin injections.
According to the Heart & Stroke Foundation, Type 1 diabetes accounts for about 5–10% of all diabetes cases in Canada. While it most commonly develops in childhood or adolescence, adults can also be diagnosed later in life.
Key features of Type 1 diabetes include:
- Sudden onset of symptoms such as frequent urination, extreme thirst, and rapid weight loss.
- Dependence on insulin therapy for life.
- Regular blood sugar monitoring to maintain stable glucose levels.
There is currently no known way to prevent Type 1 diabetes, but advances in treatment continue to improve quality of life and long-term outcomes.
Type 2 Diabetes
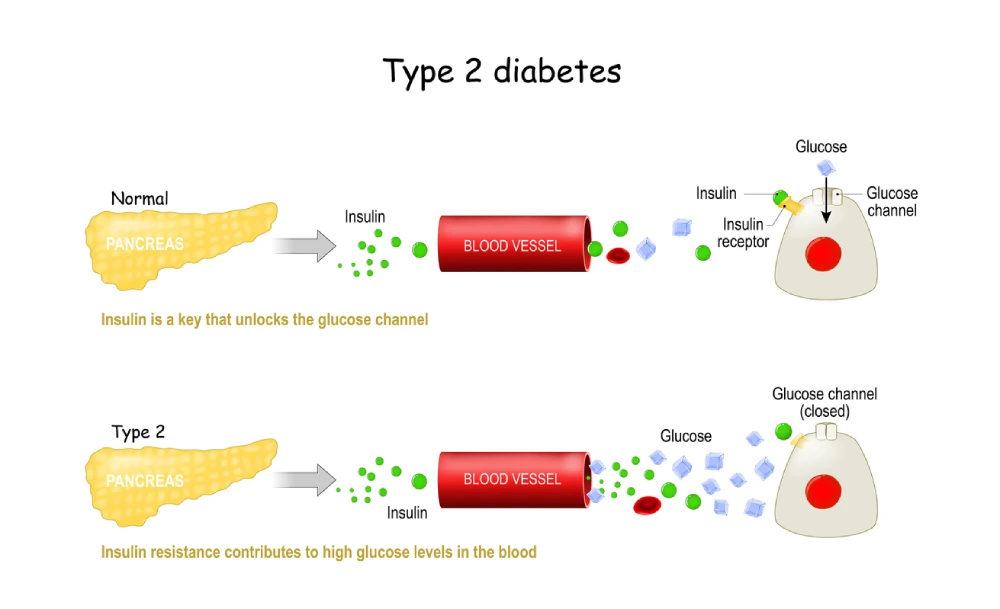
Type 2 diabetes is the most common form, representing around 90–95% of all diagnosed cases. Unlike Type 1, the pancreas still produces insulin, but the body’s cells become resistant to it, a condition known as insulin resistance.
This form of diabetes often develops gradually and may go unnoticed for years. It is typically diagnosed in adults, although cases among youth are increasing due to changes in diet and physical activity patterns.
While Type 2 diabetes has a strong genetic component, it is often linked to modifiable factors such as:
- Excess body weight, especially around the abdomen.
- Lack of regular physical activity.
- Poor dietary habits, including high intake of processed foods and sugars.
Fortunately, Type 2 diabetes can often be delayed or controlled through healthy lifestyle changes, early detection, and proper medical support.
Other Types of Diabetes
Prediabetes
Prediabetes occurs when blood sugar levels are higher than normal but not high enough for a diabetes diagnosis.
According to HealthLink BC, people with prediabetes have a higher risk of developing Type 2 diabetes, with most people diagnosed with Type 2 diabetes having had prediabetes first.
Luckily, maintaining a balanced diet and regular exercise can significantly reduce this risk.
Gestational Diabetes
Gestational diabetes develops during pregnancy when hormonal changes affect insulin function.
This condition typically resolves after childbirth, but it increases the mother’s risk of developing Type 2 diabetes later in life.
Babies born to mothers with gestational diabetes may also face higher risks of obesity or Type 2 diabetes in the future.
7 Main Causes of Diabetes: What Triggers Diabetes Development
Understanding the causes of diabetes helps identify ways to prevent or delay its onset. Here are the seven primary contributors.
1. Genetic Factors and Family History
Diabetes often runs in families. Individuals with a parent or sibling who has diabetes face a significantly higher risk. Certain genes affect how the body processes insulin or responds to glucose, making family history one of the most influential risk factors.
2. Insulin Resistance Causes
The insulin resistance that people diagnosed with Type 2 diabetes experience forces the pancreas to produce more insulin until it can no longer keep up, leading to elevated blood sugar levels. Factors that contribute to insulin resistance include obesity, inactivity, and diets high in saturated fats.
3. Autoimmune Factors (Type 1)
Type 1 diabetes develops when the immune system attacks insulin-producing beta cells in the pancreas. The cause is not fully understood, but environmental triggers and viral infections may play a role in genetically susceptible individuals.
4. Lifestyle and Dietary Factors
Diets high in refined carbohydrates, sugary drinks, and processed foods contribute to weight gain and insulin resistance. Sedentary behaviour also reduces glucose uptake by muscles, leading to elevated blood sugar levels.
5. Age and Hormonal Changes
The risk of developing Type 2 diabetes increases after age 40. In women, hormonal shifts during menopause and age-related changes in metabolism can also influence insulin sensitivity.
6. Pregnancy-Related Factors (Gestational Diabetes)
Hormonal changes during pregnancy can interfere with insulin’s ability to regulate blood sugar. It’s recommended women with gestational diabetes should be tested six weeks after giving birth, as many remain at risk for future diabetes.
7. Medical Conditions and Medications
According to Health Canada, certain health issues, such as schizophrenia, polycystic ovary syndrome (PCOS), and vascular disease, are associated with higher diabetes risk. Some medications, including steroids and antipsychotics, can also elevate blood sugar levels, leading to an increased risk.
Complications of Untreated Diabetes
If left unmanaged, diabetes can lead to serious complications affecting multiple body systems. Persistent high blood sugar damages blood vessels and nerves, interfering with daily life and long-term health.
Common complications include:
- Cardiovascular disease: Increased risk of heart attacks and strokes.
- Kidney disease: Chronic kidney failure due to overworked filtering systems.
- Neuropathy: Nerve damage causing pain, tingling, or numbness, especially in the feet.
- Vision problems: Diabetic retinopathy can cause vision loss or blindness.
Beyond the physical symptoms, unmanaged diabetes often leads to fatigue, confusion, and health-related anxiety, affecting quality of life. Early detection and consistent management can prevent or delay most complications.
Diabetes Diagnosis – How Is Diabetes Diagnosed in Canada?
Diabetes is primarily diagnosed through blood tests that measure glucose levels. These tests include:
- Fasting blood glucose test: Measures blood sugar after at least 8 hours without eating.
- A1C test: Reflects average blood sugar levels over the past 2–3 months.
- Oral glucose tolerance test: Measures how blood sugar changes after drinking a glucose solution.
In addition to lab tests, healthcare providers assess symptoms, family history, and physical health indicators such as weight and blood pressure.

Diabetes Treatment Options in Canada
Managing diabetes requires a combination of lifestyle adjustments, regular monitoring, and medical therapy tailored to each person’s needs. Effective treatment focuses on keeping blood sugar within target ranges, preventing complications, and promoting overall well-being.
Lifestyle Modifications and Diet
The foundation of diabetes care begins with lifestyle.
Following a balanced, nutrient-rich diet helps maintain healthy glucose levels. Focus on whole grains, lean proteins, vegetables, fruits, and healthy fats while limiting refined sugars and processed foods.
Regular physical activity, at least 150 minutes per week of moderate exercise, also improves insulin sensitivity and helps control weight.
Insulin Therapy
For individuals with Type 1 diabetes, and for some with advanced Type 2 diabetes, insulin therapy is essential. Different types of insulin are used based on how quickly they act and how long they last in the body:
- Rapid-acting insulins such as NovoRapid (insulin aspat) and Humalog (insulin lispro) start working within minutes and are used around mealtime to control post-meal spikes.
- Intermediate-acting insulins like Humulin-N (insulin NPH) provide longer-lasting coverage and are often used in combination with shorter-acting insulin.
- Long-acting insulins such as Tresiba (insulin degludec), Levemir (insulin detemir), and Lantus (insulin glargine) are typically taken before bed to maintain a steady baseline of insulin throughout the day.
- Mixed insulins, including Humulin 30/70 (insulin premixed 30/70), combine short- and intermediate-acting insulins for balanced control with fewer daily injections.
Your healthcare provider or pharmacist will help determine the right type and dosage, often based on your blood sugar patterns and lifestyle.
Oral and Injectable Diabetes Medications
For people with Type 2 diabetes, a variety of oral and injectable medications can help control blood sugar when lifestyle changes alone aren’t enough.
These treatments work in different ways to improve insulin function or reduce glucose levels, and are often used alone or in combination.
Some common medication types include:
- Biguanides, such as metformin
- Dipeptidyl Peptidase-4 (DPP-4) Inhibitors, like linagliptin
- Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists, such as semaglutide (Ozempic)
- Sulfonylureas, like gliclazide
- Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors, such as dapagliflozin
Your healthcare provider will choose the right option based on your blood sugar levels, overall health, and any other medications you may be taking.
Regular Healthcare Consultations
Diabetes care is most effective when supported by ongoing communication with healthcare professionals.
Regular check-ups with your doctor or pharmacist allow for medication adjustments, lab monitoring, and discussion of symptoms or side effects.
RxHealthMed pharmacists can also help you interpret glucose readings and provide personalized guidance on medication timing, storage, and administration.
Diabetes Education Programs
Across Canada, diabetes education programs offer comprehensive support for patients and families. These programs teach blood sugar monitoring, proper insulin injection techniques, foot care, and nutrition planning, empowering individuals to take control of their health and live well with diabetes.

Diabetes Prevention – How Can I Prevent Diabetes?
While not all cases of diabetes are preventable, many can be delayed or avoided with healthy habits.
Here are some proactive steps you can take to reduce your risk:
- Maintain a Healthy Weight: Even modest weight loss can significantly lower the risk of Type 2 diabetes.
- Eat a Balanced Diet: Focus on high-fibre foods, fruits, vegetables, and whole grains.
- Engage in Regular Physical Activity: Aim for 30 minutes of moderate activity most days of the week.
- Schedule Regular Health Screenings: Annual check-ups can detect early warning signs, especially if you have a family history of diabetes.
Prevention is about consistency. Small, sustainable choices make the biggest difference over time.
When Should I Call My Healthcare Provider?
Even with careful monitoring and treatment, diabetes can sometimes cause unexpected changes in your health.
Recognizing when to reach out for help is an important part of managing the condition safely. Prompt communication with your healthcare team can prevent complications and ensure your treatment plan continues to work effectively.
Contact your healthcare provider if:
- Your blood sugar levels remain consistently high or low, even after following your treatment plan.
- You experience new or worsening symptoms such as frequent urination, extreme thirst, unexplained weight loss, or vision changes.
- You notice signs of infection, foot sores, or numbness, which could signal poor circulation or nerve damage.
- You feel unusually tired, dizzy, or confused, especially if accompanied by changes in appetite or mood.
Understanding Diabetes Causes and Getting the Right Support
Diabetes is a serious but manageable condition that affects millions across Canada. Understanding the causes, from genetics and insulin resistance to lifestyle and hormonal factors, is the first step toward prevention and effective treatment.
At RxHealthMed, we’re dedicated to helping you stay informed and supported through every stage of your health journey. Our pharmacists are available to answer your questions, guide you through blood sugar monitoring, and recommend the right medications or supplies.
Ask your healthcare provider at your closest RxHealthMed pharmacy, and get the right diabetes management support and medications today.