Acid reflux is a common digestive concern that affects millions of Canadians, yet it is often misunderstood or underestimated.
When stomach acid flows back into the esophagus, it can create discomfort, disrupt daily life, and lead to more serious conditions if left unchecked. Understanding what causes acid reflux, how to recognize symptoms, and the range of available acid reflux treatment options is the first step toward lasting relief.
In this guide, we explore ways to manage acid reflux, from lifestyle strategies to effective medications. We also highlight when to seek medical attention and how your local RxHealthMed pharmacist can provide personalized support.
What Acid Reflux, Heartburn, and GERD Mean
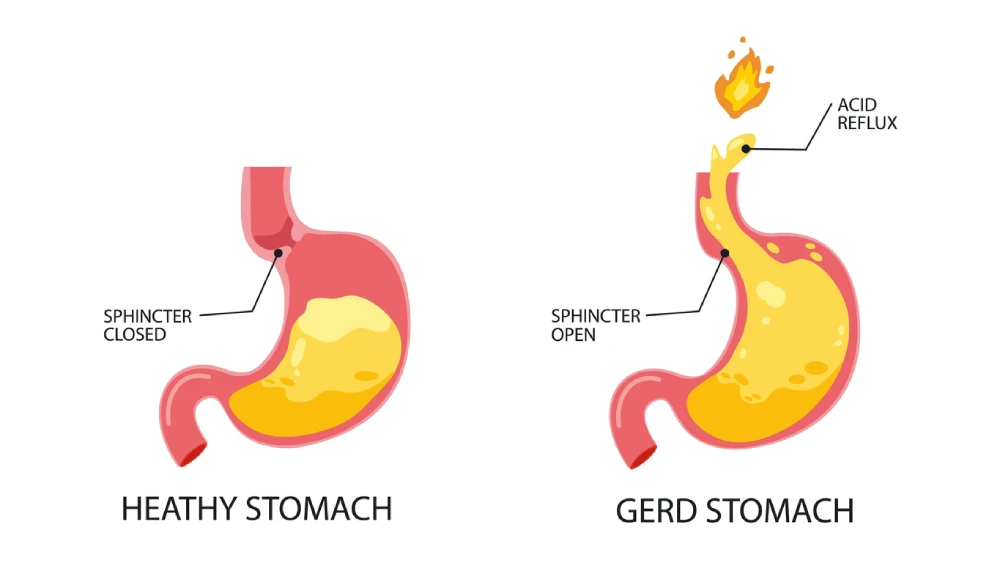
Acid reflux refers to the backward movement of stomach acid into the esophagus. Heartburn is the burning sensation many people feel behind the breastbone when this happens.
When symptoms occur frequently—more than twice a week—or when tissue damage is evident, doctors may diagnose gastroesophageal reflux disease (GERD). Although these terms are related, knowing the distinctions helps guide treatment and ensures accurate communication with healthcare providers.
Repeated acid exposure can inflame and damage the esophagus, and persistent reflux can increase the risk of complications such as esophagitis or Barrett’s esophagus, a precancerous condition.
Identifying how often you experience symptoms helps healthcare professionals decide when to recommend tests or medications.
Causes of acid reflux vary, but they typically involve a weakened lower esophageal sphincter (LES), the muscle that closes off the stomach from the esophagus.
Contributing factors include excess stomach acid, delayed stomach emptying, hiatal hernia, and certain lifestyle habits.
Understanding these underlying mechanisms can help you choose treatments that address the root cause, not just the symptoms.
Common Signs of Acid Reflux, Triggers, and Risk Factors
More than five million Canadians experience heartburn or acid regurgitation at least once a week, according to the Canadian Digestive Health Foundation. Recognizing the signs, understanding typical triggers, and knowing your personal risk factors can make management far more effective.
Acid Reflux Signs
Before beginning treatment, it is important to recognize the range of symptoms. Heartburn is the most familiar, but others can be subtle or mimic unrelated issues.
- Burning sensation behind the breastbone, often after meals
- Sour or bitter taste in the mouth caused by regurgitated acid
- Chest discomfort that may worsen when lying down
Though less common, some people may also experience a chronic cough, hoarseness, dental erosion, or difficulty swallowing.
A persistent cough or hoarseness can sometimes be the only sign, which is why evaluation by a healthcare professional is essential when symptoms linger.
Acid Reflux Common Triggers
Identifying triggers helps you prevent flare-ups before they start. While not everyone reacts the same way, research and clinical experience highlight several common culprits.
- Foods and drinks: As highlighted by Alberta Health Services, things like high-fat meals, chocolate, mint, coffee, alcohol, citrus fruits, spicy foods, garlic, and carbonated beverages often aggravate reflux.
- Timing and posture: Eating large meals, lying down within two or three hours of eating, or bending over after a meal can all worsen symptoms.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), certain blood pressure medicines, iron supplements, and bisphosphonates are known to increase reflux risk.
Acid Reflux Risk Factors
Risk factors can be short-term, long-term, or related to other health conditions. Some will also be within your control, giving you options to ease the condition with certain lifestyle changes.
- Modifiable risks: Excess weight, smoking, frequent alcohol intake, overeating, and late-night eating.
- Temporary risks: Pregnancy can increase abdominal pressure and relax the LES.
- Medical risk factors: A hiatal hernia, older age, and certain connective tissue or neurological disorders.
Knowing these risks allows you and your healthcare team to create a personalized treatment or prevention plan.
Acid Reflux Red Flags That Need Medical Care
While occasional heartburn is common, certain warning signs require prompt medical attention.
Chest pain that radiates to the arm or jaw, unexplained weight loss, persistent vomiting, or difficulty swallowing may indicate serious complications.
Acid reflux and GERD symptoms can also overlap with heart attack signs, so urgent evaluation is crucial when pain is severe or accompanied by shortness of breath, chest pain, or dizziness.
Furthermore, bleeding, whether visible in vomit or as black, tarry stools, signals potential damage to the esophagus or stomach lining.
Persistent hoarseness or a sensation of food sticking in the throat also merits investigation. If you experience these symptoms, seek care right away to rule out life-threatening conditions.
How Acid Reflux Diagnosis Works
Diagnosis begins with a detailed medical history and a discussion of your symptoms.
Healthcare providers often recommend a trial of lifestyle changes or over-the-counter medicines to see if symptoms improve. If problems persist and GERD is suspected, further testing can provide clarity.
Some diagnostic tests may include:
- Endoscopy: A flexible tube with a camera is used to inspect the esophagus and stomach for inflammation or other changes.
- pH monitoring: A small device measures acid levels over 24 hours to confirm reflux.
- Manometry: This test evaluates the function of the esophageal muscles and sphincter.
In Canada, your family physician typically coordinates these steps and may refer you to a gastroenterologist if advanced evaluation is needed.
Lifestyle Habits for Acid Reflux Relief (And Home Remedy Ideas)
Lifestyle adjustments are a cornerstone of acid reflux treatment. They not only reduce symptoms but also enhance the effectiveness of medications if required.
Eating and Drinking
Balanced eating patterns can significantly reduce reflux episodes. Some steps you can take to manage acid reflux include:
- Aiming for smaller, more frequent meals and chewing food thoroughly.
- Finishing meals at least three hours before lying down or going to bed.
- Identifying and limiting personal trigger foods such as those listed above.
Sleep and Positioning
Simple changes at night can make a dramatic difference. These include:
- Elevating the head of the bed by 15 to 20 centimetres. This helps keep stomach acid from travelling upward.
- Sleeping on the left side has been shown to reduce nighttime reflux by positioning the stomach below the esophagus.
Daily Habits
A few daily choices can support long-term relief, such as:
- Maintaining a healthy weight to reduce pressure on the abdomen.
- Quitting smoking and reducing alcohol intake.
- Reviewing current medications with your pharmacist to see if any contribute to reflux.
- Chewing sugarless gum after meals to stimulate saliva and neutralize acid.
These strategies provide a strong foundation and may help reduce or eliminate the need for continuous medication.
Acid Reflux Treatment in Canada – OTC, & Prescription Options
When lifestyle changes are not enough, a range of effective medications can bring relief. Work closely with your RxHealthMed pharmacist or physician to choose the safest and most appropriate option.
Quick Over-The-Counter (OTC) Relief
For mild or occasional symptoms, these options can help:
- Calcium carbonate antacids (such as Option+ Antacid Tablets) provide rapid but short-term relief.
- Alginates like aluminum hydroxide (liquid) or magnesium carbonate (tablet) form a protective barrier to reduce post-meal or nighttime regurgitation (such as Option+ Antacid liquid or Heartburn Relief Tablets, or Gaviscon)
- H2 blockers in low doses, such as Famotidine, can help reduce stomach acid production for several hours.
- OTC omeprazole (14-day course) is available for frequent symptoms but should not be repeated without professional guidance.
When Prescriptions Are Needed
Persistent or severe GERD may require stronger therapy:
- Higher-dose H2 blockers or proton pump inhibitors (PPIs) such as esomeprazole, omeprazole, pantoprazole, or rabeprazole, typically prescribed for 4 to 8 weeks.
- Adjustments in timing or dosage may be necessary if symptoms continue.
Pharmacist oversight is essential to ensure the correct duration and to minimize side effects.
Safe Use Guidelines
Proper use enhances benefits and reduces risks. Typical recommendations include:
- Take PPIs in the morning, 30 to 60 minutes before eating.
- Allow up to two weeks for full effect and avoid back-to-back OTC PPI courses.
- Talk to your pharmacist before using an antacid to ensure you take the proper precautions when it comes to timing, as antacids can influence the way medications or supplements are absorbed.
Long-Term Management and When to Adjust Treatment
Once symptoms are controlled, many patients can reduce or discontinue daily medication under professional supervision.
De-prescribing involves stepping down to the lowest effective dose or using medicines only as needed. Regular check-ins with your pharmacist or doctor help weigh the benefits and potential risks of long-term PPI use, including nutrient absorption concerns.
If symptoms persist despite therapy, consider adding alginates for breakthrough reflux or exploring non-acid causes such as bile reflux or motility disorders. In rare cases where medication fails and tests confirm GERD, surgical or endoscopic procedures may be appropriate.
Special Groups and Possible Complications
Certain groups require tailored management:
- Pregnancy: Lifestyle measures and safe OTC antacids are first-line. Any prescription medicine should be used only with medical guidance.
- Older adults: Medication reviews help reduce the risk of multiple medications being used to treat a condition and limit long-term PPI risks.
- Children and infants: Many outgrow reflux, but feeding strategies and careful monitoring are key.
- Active lifestyles: Athletes may need to adjust meal timing and maintain hydration to avoid reflux during activity.
 How Your Local RxHealthMed Pharmacist Helps
How Your Local RxHealthMed Pharmacist Helps
Your local RxHealthMed pharmacist is a valuable partner in managing acid reflux. We can:
- Help you create a personalized plan for over-the-counter medicines and proper timing.
- Review your current prescriptions to check for potential interactions.
- Provide guidance on when to follow up with a physician or specialist.
- Offer practical tips, such as keeping a symptom diary to track triggers and responses.
Finding Lasting Relief with Expert Pharmacy Support
Acid reflux is manageable with the right combination of lifestyle habits, targeted medications, and professional guidance.
By understanding the causes and recognizing the signs early, you can take steps to reduce discomfort and prevent complications. From simple adjustments like meal timing and sleep positioning to effective over-the-counter or prescription therapies, relief is within reach.
For trusted advice and personalized support, visit your local RxHealthMed pharmacy. Our knowledgeable pharmacists are ready to help you find safe, effective solutions tailored to your needs, so you can enjoy lasting comfort and better digestive health.
Acid Reflux FAQ
How to get rid of acid reflux?
Relief often starts with lifestyle changes such as eating smaller meals, avoiding trigger foods, and staying upright after eating. Over-the-counter antacids or H2 blockers can help if symptoms persist.
What can cause acid reflux?
Acid reflux occurs when the lower esophageal sphincter weakens or relaxes inappropriately. Contributing factors include certain foods, excess weight, pregnancy, smoking, and some medications.
How long does acid reflux last?
Occasional episodes may last a few hours, but chronic symptoms that occur more than twice a week could indicate GERD and warrant medical evaluation.





